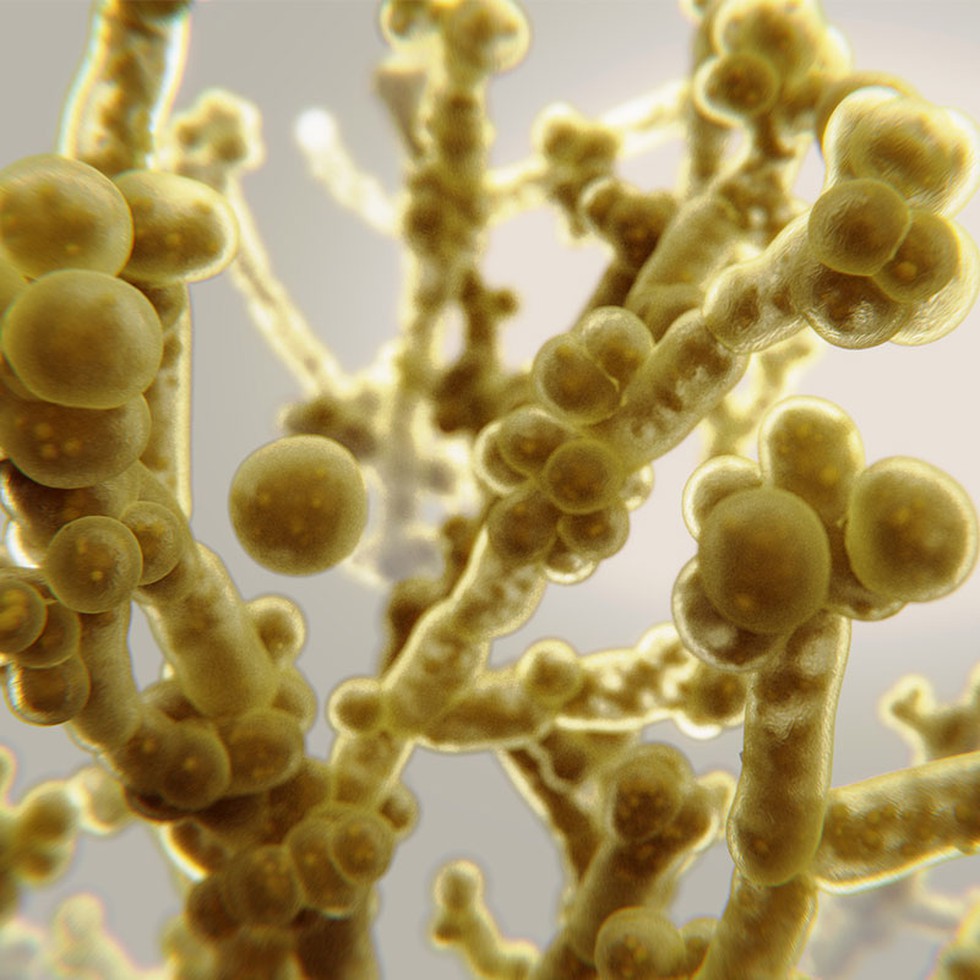
About Candida auris (C.auris):
- It is a fungal pathogen that is often multi-drug-resistant.
- This pathogen can live on the skin, inside the human body (e.g. in the gut), or in the environment.
- It is capable of causing invasive infections in the human body.
- auris causes serious infections such as bloodstream infections, meningitis, bone infections, burns/wound infections, and urinary tract infections.
- It was first identified in Japan.
- How is it contracted?
- Most cases of the fungus have been reported in healthcare settings, such as hospitals and nursing homes.
- It is generally thought to be spread through contact with contaminated surfaces or by person-to-person transmission.
- People who are already suffering from other medical conditions, recent hospital stays, and invasive devices are most at risk of contracting the fungus.
- How does the fungus act on the body? There are two ways auris can affect the body,
- The fungus can either live on a specific region, such as the skin, rectum, or mouth, in a process called “asymptomatic colonization,” where a patient has no symptoms but can spread it to other people.
- It can enter the bloodstream or wounds, where it can cause severe invasive infections.
- Symptoms:
- Its symptoms are often similar to those of other common diseases, and hence diagnosis is difficult.
- The most common symptoms of C. auris include fever and chills that don’t go away after treatment with antibiotics.
- Mortality Rate: It is estimated to be between 30-60%.
- Treatment:
- Most C. auris infections are treatable with antifungal drugs called echinocandins.
- However, some C. auris infections are resistant to the main types of antifungal medications, making them more difficult to treat.
- In this situation, multiple antifungals at high doses may be required to treat the infection.